Diagnostic Update
New factors influencing bacterial STI transmission
Syphilis and chlamydia remain significant public health concerns in Australia owing to an increase in the notification rate per 100,000 population over the last decade. The rate for Syphilis (incidences lasting less than 2 years) rose by 83% in the decade ending 2024. The chlamydia rate fluctuated, peaking at 17% before easing to 6%. 1
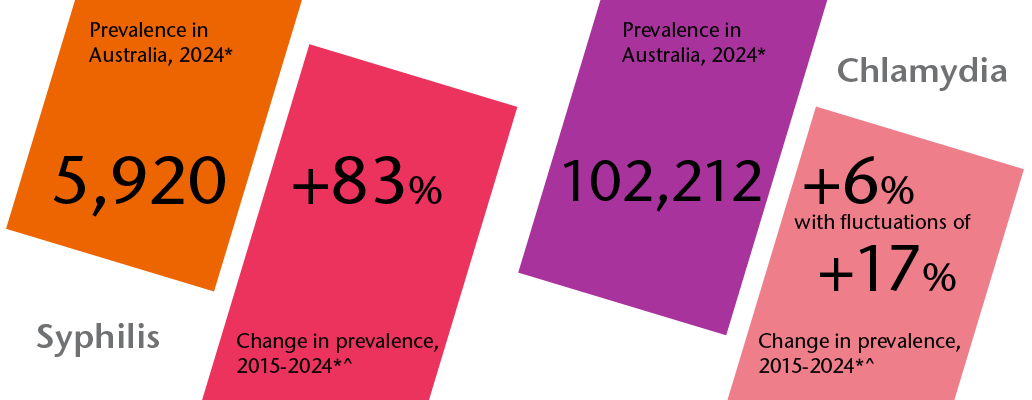
*Notifications received by the National Notifiable Disease Surveillance System (NCDSD)
# Notifications of syphilis lasting less than 2 year’s duration
^calculated by adjusted to a population of 100,000
The asymptomatic behaviour of chlamydia and other sexually transmitted infections (STI), combined with reduced access to clinical services during the pandemic, have frustrated state and territory efforts to increase screening consultations and lower diagnoses. 2
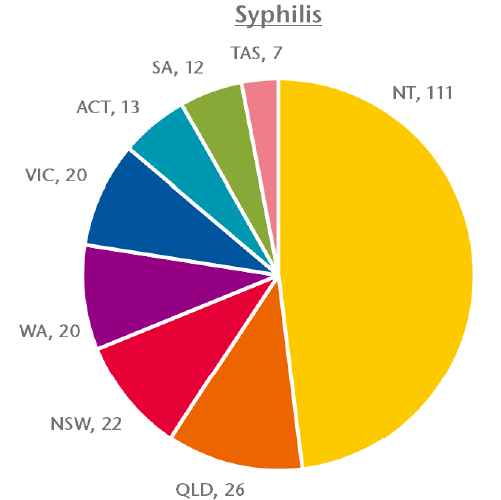
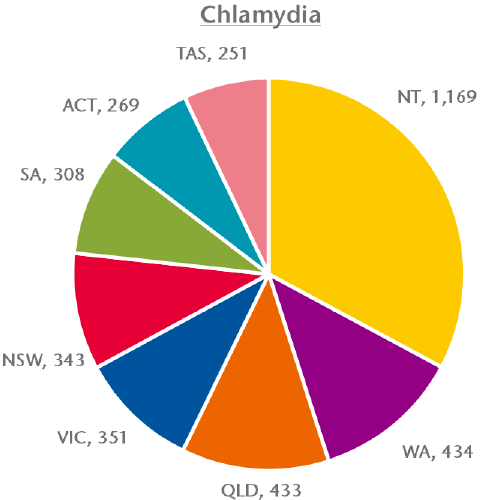
Notifications per 100,000 population (2024)
The stubborn increases in chlamydia and syphilis diagnoses have motivated the development of new tools and guidelines targeting the highest-risk communities. These new factors are likely to profoundly influence the prevalence of both infections, care-seeking behaviours, and diagnostic priorities in Australia.
Care-seeking behaviour of the LGBTQIA+ community
Learnings from HIV
Clinical attitudes toward gay, bisexual and other men who have sex with men (GBMSM), are often limited to stigma of promiscuity and other risk-taking behaviours. Stigmatisation has culturally centred upon human immunodeficiency virus (HIV) transmission. The reality for GBMSM is a triumphant decline in HIV notifications. Diagnoses declined by 64% for Australian GBMSM in the decade ending 2023, compared to the national 33% decline. 3
The decline in HIV can be traced to improved access to sexual health screening for GBMSM, the implementation of point of care (POC) testing, and targeted marketing campaigns to increase the frequency of testing and mitigate testing stigma. Importantly, the queer community delivered cultural change in care-seeking and risk-taking behaviour to uphold their responsibility to manage HIV transmission.
Since its introduction to the Pharmaceutical Benefits Scheme (PBS) in 2018, pre-exposure prophylaxis (PrEP) empowered at-risk cohorts including GBMSM to significantly reduce the probability of contracting HIV if exposed. Users of PrEP via PBS who had been prescribed in the past 12 months peaked at 47,172 in Q2 2024, accounting for 59% of the cumulative total. 4

The once-daily preventative medication, alongside on-demand methods, was a public test of diligence and vigilance for the Australian queer community that was closely scrutinised by epidemiologists and clinical guideline authorities. 5
Combatting Bacterial STIs
Doxycycline post-exposure prophylaxis (Doxy-PEP) is a new medication to mitigate transmission of bacterial STIs.
Doxy-PEP was recently introduced to the Australian GBMSM community following a consensus statement in 2023, informed by post-market surveillance data findings from the USA and other countries. Unlike PrEP, a doxy-PEP dose is to be administered within 72 hours after high-risk sexual activity. 6
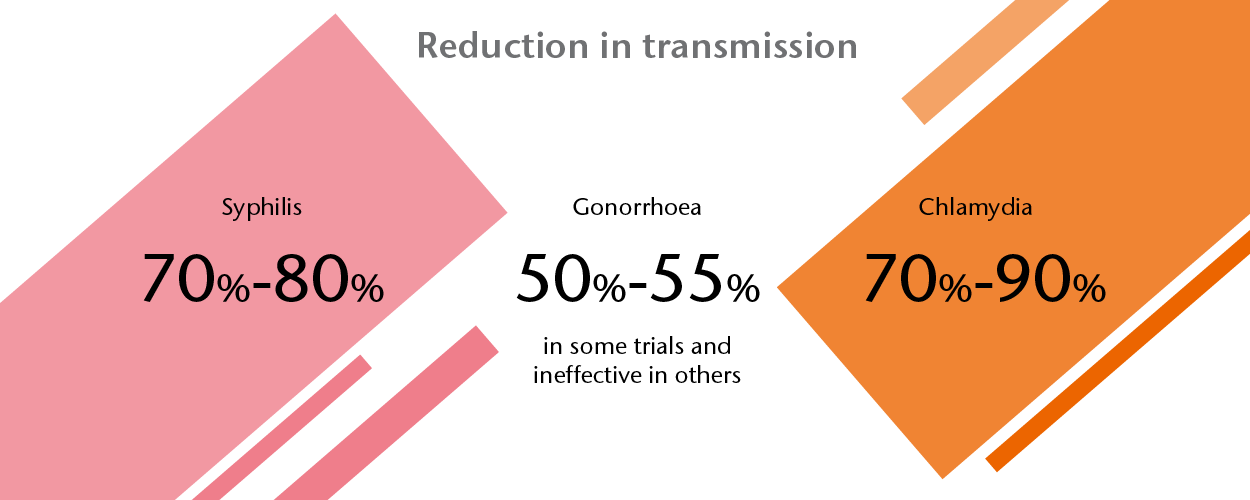
Initially hoped to target all bacterial STIs, the Australian consensus statement on doxy-PEP only recommended doxy-PEP for the primary purpose of targeting syphilis transmission, with secondary benefits against chlamydia and gonorrhoea. 8
The tiered prioritisation of STI targeting with doxy-PEP is chiefly due to antimicrobial resistance (AMR), particularly the elevated incidences of tetracycline resistance in Australian gonococcal isolates. The rate of gonococcal tetracycline resistance is 41% in Australia, with the highest incidence in Victoria at 51%. 9
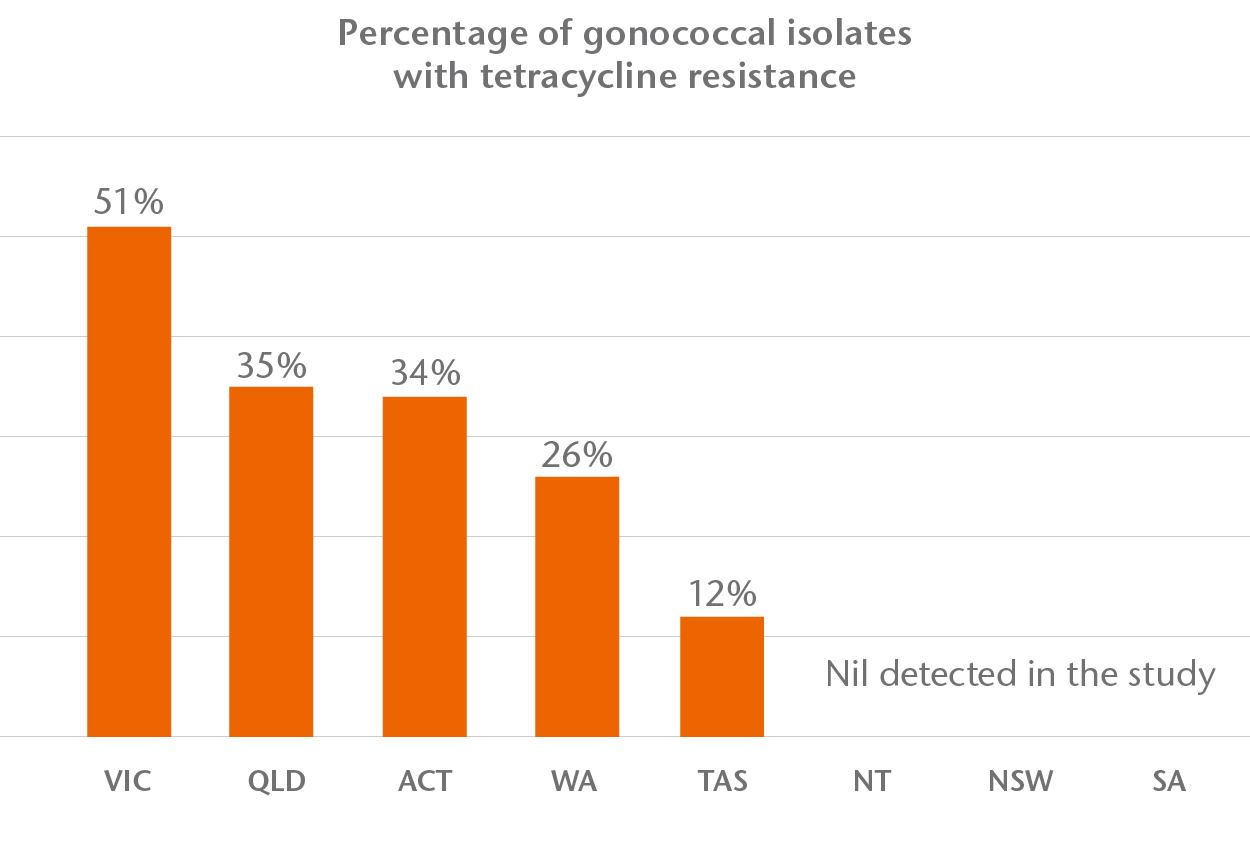
Although tetracycline resistance in Australian gonococcal isolates is high, tetracycline is not a standard treatment for gonorrhoea in Australia. The effect on AMR of doxy-PEP usage against resistant Neisseria gonorrhoeae is not well understood. 8
Despite the intrusive lifestyle effects demanded by doxy-PEP usage, the queer community’s ability to reduce HIV diagnoses when empowered with PrEP lends promising feelings towards the future of doxy-PEP and its successors. However, the issue of antimicrobial stewardship suggests that clinicians should expect a more complicated diagnostic landscape as doxy-PEP uptake improves. Doxy-PEP represents a need for a cooperative intersection between the diagnostics industry and preventative medicine design. 10
The future of sexual health screening in Australia
With the looming unpredictability for the future of AMR in Australia and the anticipated increase in doxy-PEP uptake, AMR screening may need to be integrated into routine screening to complement STI detection to ensure antimicrobial stewardship and effectively manage the genetic diversity of bacterial STIs.
Multiplexed syndromic screening is the ideal tool to seamlessly combine detection of pathogens that cause bacterial STIs and their AMR genetic markers.
Detection of pathogens and AMR can be combined in various ways to suit laboratory through-put requirements and budgets. Simultaneous screening assures maximum convenience for technical staff with minimal time to patient intervention. Tandem screening, with pathogen detection preceding AMR screening for positive samples, offers the benefit of improved throughput of samples when STI prevalence is low. Tandem screening also reduces reagent waste of superfluous AMR tests without compromising the highest level of vigilance. A hybrid process may be preferable in an environment with unpredictable STI prevalence, in which tandem screening is used during periods with lower sample positivity rates and switching to simultaneous screening when rates increase beyond a calculated threshold.
For additional information about this article, please reach out to media@r-biopharm.com.au
References
- Department of Health and Aged Care. “National Communicable Disease Surveillance Dashboard”. Accessed March 2025. https://nindss.health.gov.au/pbi-dashboard/
- Chow, Eric PF, Jane S. Hocking, Jason J. Ong, Tiffany R. Phillips, and Christopher K. Fairley. “Sexually transmitted infection diagnoses and access to a sexual health service before and after the national lockdown for COVID-19 in Melbourne, Australia”. In Open Forum Infectious Diseases, vol. 8, no. 1, p. ofaa536. US: Oxford University Press, 2021. https://academic.oup.com/ofid/article-pdf/8/1/ofaa536/36218526/ofaa536.pdf
- UNSW Kirby Institute. “HIV diagnoses trending down in Australia despite 2023 increase”. Accessed March 2025. https://www.kirby.unsw.edu.au/news/hiv-diagnoses-trending-down-australia-despite-2023-increase
- UNSW Kirby Institute. “Monitoring HIV pre-exposure prophylaxis (PrEP) uptake in Australia”. Issue 11, 2024. https://www.kirby.unsw.edu.au/sites/default/files/documents/Monitoring-HIV-pre-exposure-prohpylaxis-PrEP-uptake-in-Australia_Issue-11.pdf
- UNSW Kirby Institute. “HIV Data”. Accessed March 2025. https://www.data.kirby.unsw.edu.au/hiv
- Cornelisse, Vincent J., Benjamin Riley, and Nicholas A. Medland. “Australian consensus statement on doxycycline post‐exposure prophylaxis (doxy‐PEP) for the prevention of syphilis, chlamydia and gonorrhoea among gay, bisexual and other men who have sex with men.” Medical Journal of Australia 220, no. 7 (2024): 381-386. https://pubmed.ncbi.nlm.nih.gov/38479437/
- Cornelisse, Vincent J., Jason J. Ong, Nathan Ryder, Catriona Ooi, Arthur Wong, Penny Kenchington, Massimo Giola et al. “Interim position statement on doxycycline post-exposure prophylaxis (Doxy-PEP) for the prevention of bacterial sexually transmissible infections in Australia and Aotearoa New Zealand–the Australasian Society for HIV, Viral Hepatitis and Sexual Health Medicine (ASHM).” Sexual health 20, no. 2 (2023): 99-104. https://www.publish.csiro.au/SH/pdf/SH23011
- Cornelisse, Vincent J., Benjamin Riley, and Nicholas A. Medland. “Australian consensus statement on doxycycline post‐exposure prophylaxis (doxy‐PEP) for the prevention of syphilis, chlamydia and gonorrhoea among gay, bisexual and other men who have sex with men.” Medical Journal of Australia 220, no. 7 (2024): 381-386. https://onlinelibrary.wiley.com/doi/pdfdirect/10.5694/mja2.52258
- Lahra, Monica M., Tiffany R. Hogan, and Benjamin H. Armstrong. “Australian gonococcal surveillance programme annual report, 2021.” (2022). https://www1.health.gov.au/internet/main/publishing.nsf/Content/2A15CD097063EF40CA2587CE008354F1/$File/australian_gonococcal_surveillance_programme_annual_report_2021.pdf
- Ehsan, Rifa, Alexa B. D’Angelo, Drew A. Westmoreland, and Christian Grov. “Perceptions about doxycycline post-exposure prophylaxis (Doxy-PEP) as an STI-prevention strategy among gay and bisexual men (GBM) in the United States: Results from a qualitative study.” Preventive Medicine 183 (2024): 107977. https://www.sciencedirect.com/science/article/abs/pii/S0091743524001324
News & Media
Posted in Diagnostic Updates
